When Eric Wood talks about the future of college mental health, he does so from the front lines. The longtime director of Texas Christian University’s Counseling and Mental Health Center and past president of the Texas University and College Counseling Directors Association has just been elected the next president of the Association for University and College Counseling Center Directors (A.U.C.C.C.D.). His tenure will begin in October 2026.
Known for his innovative Comprehensive Collaborative Care Model and award-winning e-book, “A New Narrative for College Mental Health,” Wood is stepping in to lead the nation’s largest organization for campus counseling leaders at a moment when the field, like all of higher ed, is confronting change. We caught up with him fresh off hosting a national symposium on performing artists and athletes and took the opportunity to ask him about A.U.C.C.C.D.’s plans and priorities.
LW: Congratulations on your election as president-elect of A.U.C.C.C.D. What do you see as the major challenges for the organization in the coming year?
EW: We as counseling centers have done a really good job capturing the narrative of how important college mental health is. College mental health has a lot more significance than people realize. If you think about the demographic we serve, the traditional 18- to 25-year-olds, that’s a prime demographic for pretty much anything — substance use, suicide, emerging disorders. It’s also the best time to treat them because if you can treat them then, they may have fewer episodes later, or none at all. Whereas if they wait 10 or 15 years, it’s a lot more ingrained and harder to treat.
Colleges and universities have greater access to that demographic than any other health-care system. They live, walk by, and travel by our campuses every day. So the question is: What opportunities does that create if government and other organizations really recognize this?
LW: You’ve become known for T.C.U.’s innovative model of collaborative care. Can you explain what that is and how it ties into your national leadership goals?
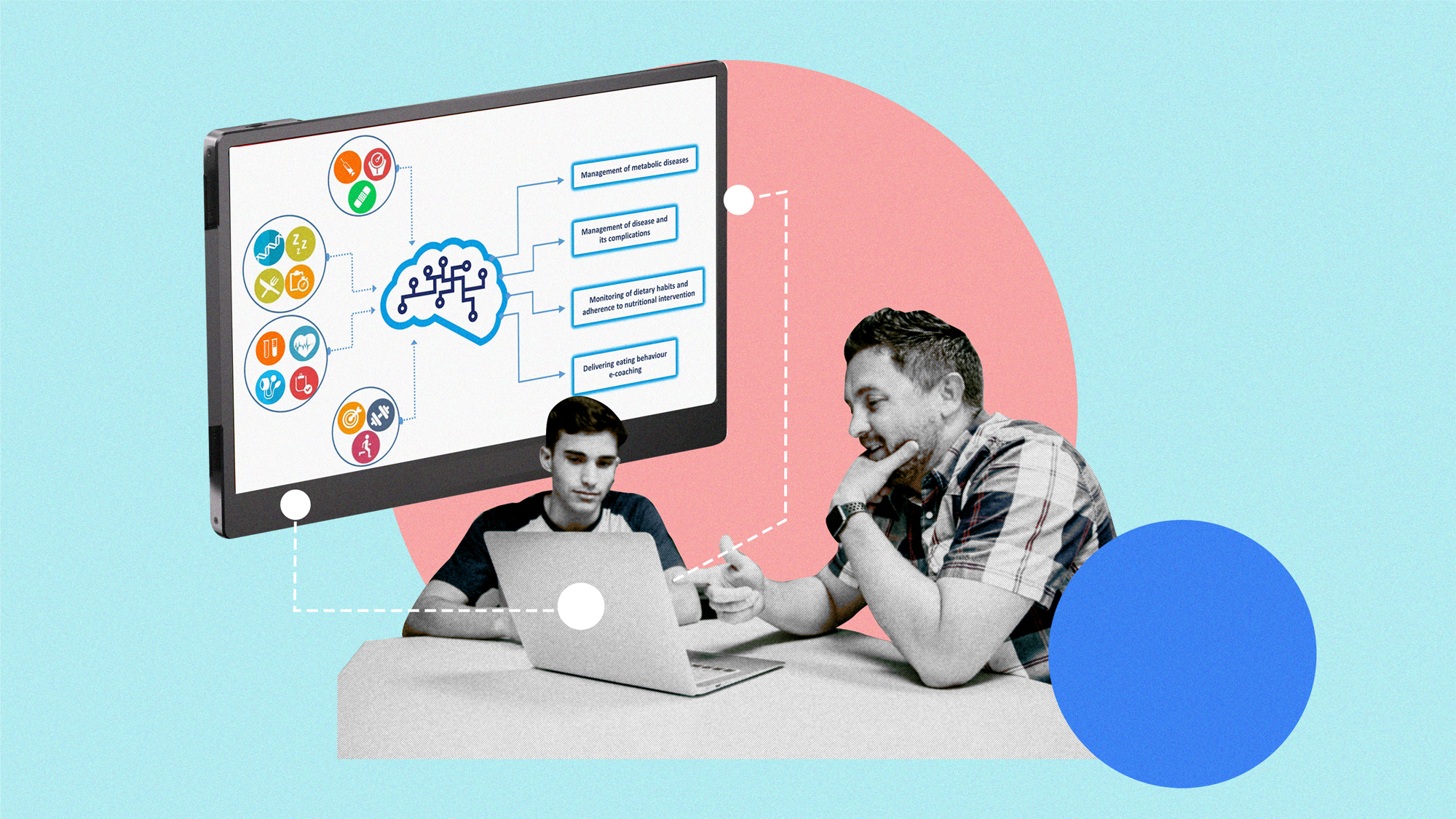
EW: We call it the Comprehensive Collaborative Care Model, and it’s reshaping how universities think about their role in mental health. We started it during the pandemic. The mindset had always been that college counseling centers were designed for developmental concerns — the stress that comes from change — not necessarily for students with high mental health needs. But those dynamics have shifted. Now we have students with much higher needs, and our systems weren’t designed for that.
So instead of building hospital-style treatment centers, we built bridges. We partner with community providers who were designed to work with individuals with high needs but who lack the infrastructure and access we have. They come onto our campus, use their programs, and our students stay in school, on our campus, in programs with other college students. It’s a win-win-win: The student’s insurance covers most costs so there’s just the co-pay, and we’ve gotten grants and donors so the treatment centers have the chance for little or no overhead. We’ve trained over 100 schools to replicate various parts of the model.
LW: You mentioned that politics and policy changes are affecting mental health care on campuses. What are you seeing?
EW: If you’re in a university that’s depending on federal funding, there’s a new level of raised exposure. There’s a perception that if a state or federal funding source doesn’t like something at your institution, they’re going to cut your funding off. People don’t realize that even if it had nothing to do with college counseling centers, it is going to trickle down if schools have that cut in funding. When universities face federal or state funding cuts, that trickles down to us. A 20 percent budget cut across campus means a 20 percent cut for the counseling center, too. And yet the demand for services has never been higher.
A lot of the culture-war legislation, like D.E.I. bans, has had unintended consequences. Some states have medical exemptions for those laws, but others don’t. We’ve seen schools cut services that were never meant to be targeted, like gender specific groups with mental health and addiction issues. This is an age group much more likely to seek help on campus than they would after graduation, so when you remove those options, you lose opportunities to intervene early.
“When policymakers pass laws or set funding priorities, I hope they think carefully about how that affects college mental health.”
We’re trying to make lawmakers aware that mental health has never been a partisan issue. Surveys show eight out of ten Americans believe schools are responsible for providing health care to students. The narrative we’re pushing is: “Look at the possibilities higher education offers society. Why would you want to limit that potential?”
LW: What other issues are most pressing for college counseling centers right now?
EW: We’re still seeing the ripple effects of the pandemic. And we do know that in this age group one of the things that spiked is their likelihood to transfer. The students entering college now were in middle school during the shutdowns — the classes of 2028 through 2030. That’s a critical cohort with a lot of struggles. They missed key developmental years, and those formative years had a lot of disruption going from middle school to high school, and we see that in their social and academic adjustment carrying over to higher education.
And as digital natives engaged in all the social platforms, they’re used to absorbing all the culture and content and polarizations in society. That’s their reference point, and a lot of them may not know what it’s like to not have that level of polarization. So they’re bringing that to campus. When they see politicians saying certain words or treating each other some way, you’re going to see that carry over to how they treat faculty. They see that people just break rules; you see that happening in politics and society, and that carries over into the res halls because that’s the frame of reference.
We’re also seeing a higher level of parental involvement. Their parents spent more time with them during lockdowns, engaged in a closer front-row seat to their education, so now we’re seeing that continue — sometimes helicopter-level involvement — in college life.
LW: What’s on your personal wish list as incoming president?
EW: To keep building that narrative and have a stronger voice nationally. We’ve had some success getting attention from politicians and national outlets, but there’s so much more to do. When policymakers pass laws or set funding priorities, I hope they think carefully about how that affects college mental health.
And college is where the developmental concerns play out because this is the prime age. The reason why colleges created counseling centers wasn’t because we thought every student had a clinical diagnosis. Most students do not. The centers exist because we define stress as heightened in times of major change, and a major one is when you start college. You only have about four or five of those moments in your life when everything can change. So starting college is one of them — you change where you eat, where you live, your identity, everything — and then graduating college is a second one. So you have so much change bookmarking the college experience. And then you do have associated stressors, like navigating the social environment, and we know that demographic tends to engage in high-risk behavior, so a lot of prevention work is important. That is why college counseling centers exist, and I contend colleges and universities are the best in the world at doing that. But because there’s currently a lot more students with high mental health needs coming to campus, the disconnect occurs that we aren’t good at what we’re doing. That couldn’t be further from the truth.
The mental health of young people is always going to be a popular, bipartisan cause. We just need to remind people of that and continue the collaboration.
LW: How do you see that collaboration playing out at the national level?
EW: Collaboration is essential. Some states have strong organizations, like Texas, but not all do. One of my goals is to help develop those networks. State laws affect us differently, so we need local collaboration as well as national unity. There’s strength in numbers, whether it’s state collectives, regional conferences, or collaborations across university systems, like the athletic conferences.
It’s also about mutual support. A lot of what’s in the headlines about higher education doesn’t directly involve counseling directors, but it still affects us through funding cuts, political pressures, or staffing shortages. Directors need to come together because having a collaborative amplifies our method, our messages. We need each other to stay resilient.
LW: You just hosted a symposium on athletes and performing arts. What can you tell us about the thinking behind spotlighting those populations?
EW: It really came out of conversations we were having on our campus about performing artists and athletes — two groups that represent the university in powerful ways but have very different kinds of support systems. Varsity athletes get a lot of institutional support, but there are just as many performers and non-varsity athletes who face similar pressures and injuries without the same safety nets.
For example, if a student athlete gets hurt, the university often covers the care, and they can still progress toward their degree. But if a dancer or musician gets injured, they often can’t progress toward their degree because performance is part of their coursework. That difference really highlights why universities need to think more broadly about how they support these students.
So we decided to organize a symposium to explore that. We reached out to experts from Johns Hopkins, Stanford, Harvard — literally the pioneers of performing arts medicine — and every single one of them said yes. We even had ballerina Tiler Peck as a keynote. It turned into a two-day virtual event that drew about 100 sign-ons per session; many of them were in classrooms watching together. It was the first time we’d done anything like it, and it really underscored how much synergy there is between athletic and performing-arts wellness.
LW: How long have you been at T.C.U., and what do you think your election says about A.U.C.C.C.D. and where it’s headed?
EW: I started at T.C.U. right out of my Ph.D. program in 2007 and became director in 2019, so I had one good semester before the pandemic hit. Everything we’ve built since then has been about adapting to change and meeting students where they are.
I’m honored by the role. I think part of the reason I was elected is because we’ve done a good job at innovation at T.C.U., and I think it shows a shift in the narrative about college mental health. For a long time, the assumption was that we as colleges were limited — that if a student had a serious mental health disorder, they needed to go elsewhere, just like you wouldn’t expect a university to perform surgery. But that’s changing. For example, one of our specialized programs is an intensive outpatient program on campus. I’d love to see every residential campus in America have one. The impact would be generational.
So, I think my election signals that people are starting to recognize the potential and the possibilities of what we can do — and that we can do it at a fraction of the cost, using programs that already exist. And why would you want to do anything to ruin that potential? To have my colleagues across the country say, “We want that kind of innovation leading us forward” — that’s deeply meaningful. It tells me people see the potential of college mental health, and they’re ready to invest in it.